Study shows the role of a redox protein in arterial hypertension
Arterial hypertension, a disease that affects more than 30% of the world’s adult population, is associated with endothelial dysfunction, which is characterized by an imbalance in the release of contractile and relaxing factors, with increased production of reactive oxygen species to the detriment of nitric oxide. The main source of the superoxide free radical in vascular cells is the enzyme NADPH oxidase 1 (Nox1), which can be activated in response to several factors, including protein disulfide isomerase A1 (PDIA1).
In a paper published in the Journal of Hypertension, researchers from the RIDC Redoxoma led by professor Lucia Rossetti Lopes from the Instituto de Ciências Biomédicas at the Universidade de São Paulo (USP) have shown that PDI plays an important role in the pathogenesis of hypertension via regulating transcription factor ATF1-induced Nox1 gene expression and calcium mobilization, which increases vascular tone and contributes to blood pressure elevation. Previously, the authors identified PDI as a new protein that regulates Nox1 signaling in vascular smooth muscle cells (VSMCs).
“We now showed how the regulation of PDI happens at the transcriptional level: it acts on the Nox1 gene, regulating the gene expression of the enzyme. The beauty of this work is that we investigated signaling in cells and then tested the functional effect on the vessel, in arteries of spontaneously hypertensive rats. It’s a complete study.” said Lucia Lopes.
PDIA1, or just PDI, is the prototype of the PDI family, which belongs to the thioredoxin superfamily. It is a ubiquitous protein essential for the survival of our cells, with important physiological functions. PDI participates in signaling and redox homeostasis. Its classic function is to catalyze the insertion of disulfide bonds into nascent proteins in the endoplasmic reticulum (ER), ensuring their correct folding.
The relationship between PDI and the production of oxidants involves NADPH oxidase (Nox), a family of enzymes that catalyzes the reduction of molecular oxygen, generating the superoxide radical anion, which, in turn, participates in the generation of other oxidants. In the human vasculature, several members of the Nox family control physiological functions such as growth, migration, and extracellular matrix modifications in vascular smooth muscle cells (VSMCs). Noxs are also involved in the regulation of vascular tone. They are distributed throughout the vessel wall, and particularly Nox1 is involved in the migration of VSMCs from the medial layer to the intima, contributing to the formation of neointima, vascular stenosis, and increased blood pressure.
Results
Comparing vascular smooth muscle cells (VSMCs) from spontaneously hypertensive rats with cells from control Wistar rats, the researchers found that PDI increases the transcription of Nox1 through the activation of the epidermal growth factor receptor (EGFR), responsible for cell signaling, proliferation, migration, and contraction. PDI also promotes the transport of the transcription factor ATF1 to the cell nucleus. When investigating the region of the Nox1 gene with which ATF1 associates, they discovered that it binds to enhancers, which are sequences that increase gene expression.
“The increase in Nox1 activity, that is, the increase in superoxide production, activates the metalloprotease that cleaves the Hb-EGF ligand. This, in turn, activates the EGRF receptor, which activates the ATF1 transcription factor via ERK 1/2 signaling. ATF1 then migrates to the nucleus, where it increases the expression of Nox1, which goes to the membrane,” Lopes explained.
Furthermore, they showed for the first time that PDI sulfenylation by hydrogen peroxide contributes to EGFR activation in hypertension. PDI sulfenylation was higher in cells from spontaneously hypertensive rats than in control animals, suggesting higher oxidation of PDI in high blood pressure.
PDI silencing or pharmacological inhibition in vascular smooth muscle cells significantly decreased EGFR activation and Nox1 transcription. Overexpression of the protein increased ANG II-induced EGFR activation and ATF1 translocation to the nucleus.
To investigate whether the modulation of Nox1 signaling by PDI translated into functional responses, the researchers evaluated the contractile response to angiotensin II in peripheral resistance arteries of spontaneously hypertensive rats. They concluded that PDI increases intracellular calcium mobilization and ANG II responses in these arteries. “Unlike most studies that use cells from the aorta, which are conductance vessels, we used cells from the mesenteric arteries of these animals. These arteries have a smaller caliber; thus they are resistance vessels,” said the researcher.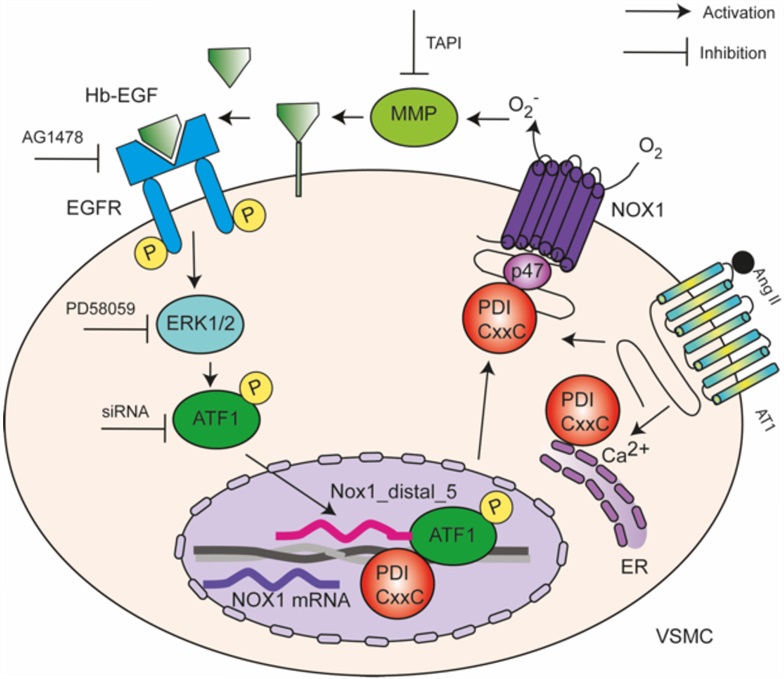
Therapeutic Target
Arterial hypertension, called the “silent disease” because it does not present obvious symptoms, is a risk factor for stroke, aneurysm, myocardial infarction, and chronic kidney disease. “As we age, the arteries become stiffer, they respond less to expansion/contraction, becoming less elastic. This is one of the characteristics that will make the disease appear more in the elderly population,” said Lopes.
In the article, the researchers show a clear correlation between increased Nox 1 expression, PDI, and blood pressure. “That’s why I think it has some therapeutic potential. Currently, the main medications we use to treat high blood pressure are ACE inhibitors, which inhibit the formation of angiotensin II, one of the main activators of Nox 1. ACE inhibitors indicate that the mechanism we have revealed may indeed be a therapeutic target.”
The big question, according to the researcher, would be to discover a new class of drugs with greater specificity and, therefore, fewer side effects. “We would have to look for inhibitors that could inhibit downstream from the AT1 receptor, that were more specific. PDI could offer a way to do that.“
The article Protein disulfide isomerase-mediated transcriptional upregulation of Nox1 contributes to vascular dysfunction in hypertension, by Livia De Lucca Camargo, Silvia Cellone Trevelin, Guilherme Henrique Gatti da Silva, Ana Alice dos Santos Dias, Maria Aparecida Oliveira, Olga Mikhaylichenko, Aline C.D. Androwiki, Celio Xavier dos Santos, Lisa-Marie Holbrook, Graziela Scalianti Ceravolo, Alexandre Denadai-Souza, Izabela Martina Ramos Ribeiro, Simone Sartoretto, Francisco Rafael Martins Laurindo, Patricia Pereira Coltrl, Vagner Roberto Antunes, Rhian Touyz, Francis J. Miller Jr., Ajay M. Shah, and Lucia Rossetti Lopes, can be accessed here.
