Endogenous photosensitizers are crucial for the action of UV-A and visible light on human skin, shows review
No matter which part of the human body is exposed to light - hair, skin, or eyes - or whether the light source is natural or artificial, the biological consequences of light-induced oxidation reactions largely depend on the intrinsic photochemical properties and location of photosensitizers naturally present in biological tissues, called endogenous photosensitizers, which are molecules that transform light energy into chemical reactivity.
When we sunbathe, the endogenous photosensitizers in our skin cause both beneficial and harmful transformations. In a review article published this week in the prestigious journal Chemical Reviews, scientists Erick L. Bastos, Frank H. Quina, and Maurício S. Baptista, from the Instituto de Química, Universidade de São Paulo (USP) present a comprehensive analysis of endogenous photosensitizers in human skin, investigating the connections between their electronic excitation and the subsequent activation or damage of biomolecules. The work reveals the possible causes of the continued increase in global cases of skin cancer and points out the limitations of current sun protection approaches.
“We were able to position the frontier of the photochemistry that takes place in the skin under sun exposure. We show the photosensitizers and the reactions. We talk about proteins, lipids, carbohydrates, and everything else relevant to the topic. It is an important paper both for its scope and depth, and the chemical formalism is perfect. I expect that this work will encourage further research in this area”, said Maurício Baptista, also a member of the RIDC Redoxoma.
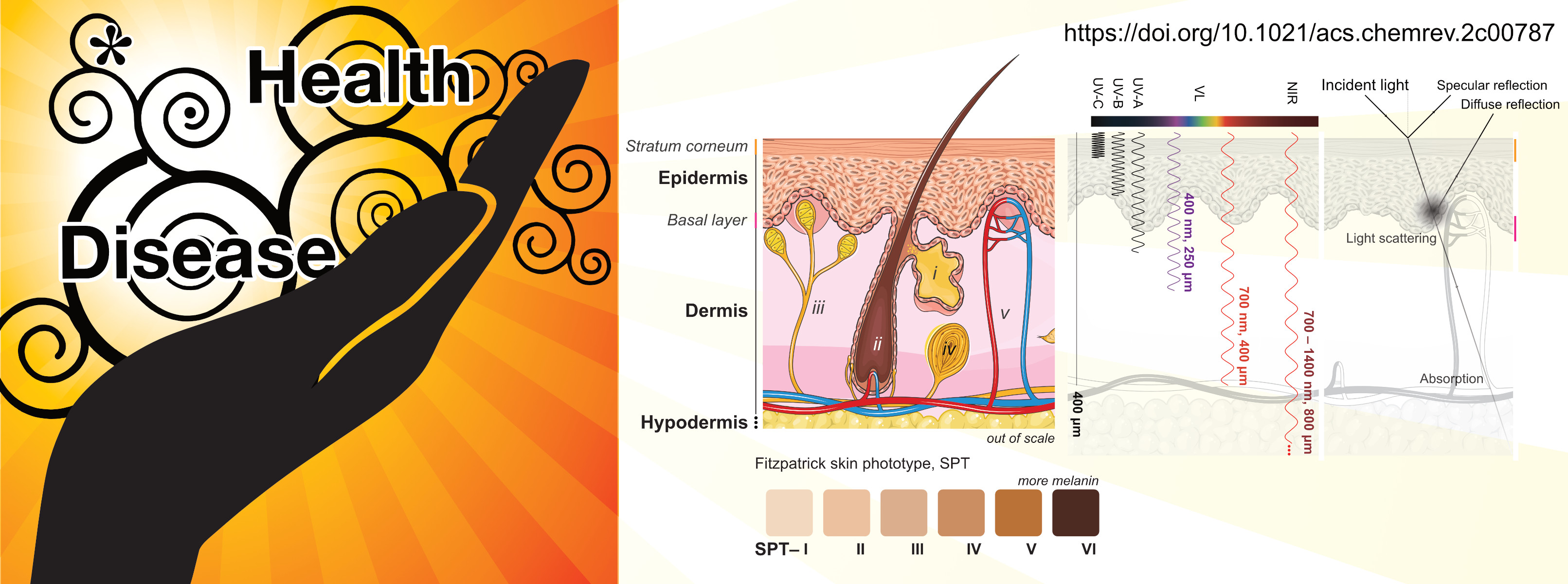
The skin is made up of three layers: epidermis, dermis, and hypodermis. Light reaches different depths into the skin, depending on the length of the radiation, the characteristics of the absorbing species present, and the optical properties of the skin. Ultraviolet B (UV-B) rays, which represent about 5% of the UV radiation that reaches Earth, penetrate only the most superficial layers of the skin (epidermis), barely reaching the dermis. Ultraviolet A (UV-A) rays and visible light reach the basal cell layer and the dermis and are absorbed by endogenous photosensitizers.
Visible light represents about 47% of the total solar radiation that reaches human skin and is the spectral range that forms the highest levels of free radicals generated in the skin under sun exposure, accounting for 50% of the total.
Photosensitization
Although UV-B radiation is considered more deleterious because it is absorbed directly by DNA, the researchers say that an important message from this review is that photosensitization allows visible light and UV-A radiation to produce large effects on the skin. Photosensitized oxidations are reactions caused by the interaction of light with a photosensitizing molecule in the presence of oxygen.
Photosensitizers are present in specific concentrations and locations and include small molecules, such as vitamins, amino acids, and cofactors, and macromolecules, such as proteins, nucleic acids, and glycans. In the presence of molecular oxygen, they absorb radiation and generate reactive oxidants, such as triplet excited species, and those derived from oxygen itself, such as singlet oxygen, superoxide radical, and other reactive species derived from them. What these molecules are and what reactions they are involved in after absorbing solar radiation are issues discussed in unprecedented depth in this review. Thus, according to the researchers, this article should also serve as a reference source for information that today is spread across hundreds of articles in the scientific literature.
Biological responses to excessive sun exposure, such as apoptosis (programmed cell death), sunburn, hyperproliferation, and mutation, are initiated both by direct damage to DNA nucleobases, in particular by the formation of cyclobutane pyrimidine dimers (CPDs), and by indirect damages caused by the oxidation of these nucleobases or other molecules important for cell survival.
Indeed, cells will survive or die depending on the extent of damage done to their major intracellular components such as mitochondria, endoplasmic reticulum, and lysosomes. Even low concentrations of efficient photosensitizers such as methylene blue and crystal violet trigger different forms of regulated cell death by affecting these cellular components. This means that the effects of radiation depend not only on the intrinsic photochemical properties of the photosensitizers but also on their location.
UV-A radiation causes both direct photodamage and photosensitized oxidation reactions, that can compromise the viability of cells located much deeper in the skin and eyes. This can occur by several mechanisms, including lipid peroxidation, DNA damage, and activation of pro-inflammatory signaling pathways, leading to cellular dysfunction, inflammation, and potentially increased risk of skin and ocular disorders such as actinic keratosis, photoaging, basal cell carcinoma, carcinoma squamous cell disease, cataracts, and age-related macular degeneration.
Visible light, particularly in the violet-to-blue interval, also targets endogenous photosensitizers in the dermis and even deeper tissues and organs in the body, potentially leading to DNA damage. Even melanin, the pigment responsible for skin color and protection against UVB rays, can cause oxidative stress and indirect damage to DNA in photosensitization reactions induced by visible light. “Interestingly, light also can treat illnesses, and because it penetrates deeper into the skin, visible light is now used to treat many illnesses”, Baptista says.
Two mistakes
“In terms of public health, there are two main problems with guidance on sun exposure: it is misleading to say that people can use sunscreen and stay in the sun for a long time; and, on the other hand, it is also a mistake to say that the sun is always dangerous, in any condition”, says the researcher.
On the sun’s beneficial aspects for health, he mentions a controlled study with approximately 30,000 women without a history of cancer, randomly chosen from the Swedish population, which found that low exposure to the sun is a risk factor for all-cause mortality. “Few things studied increase or decrease life span with statistical significance. The sun is one of them.“
Vitamin D activation, for example, depends on intracellular reactions initiated by the absorption of UV-B photons by 7-dehydrocholesterol. This process has many beneficial biological consequences, including regulation of calcium homeostasis and bone metabolism, inhibition of tumor cell proliferation, and prevention of autoimmune and cardiovascular diseases. In addition, mainly UV-B and UV-A radiation, but also less efficient blue light can promote the release of nitric oxide, contributing to systemic blood pressure reduction through vasodilation, control of macrophage cytotoxicity, and stimulation of wound healing.
According to the researchers, the habit of spending time indoors and avoiding exposure to the sun resulted in an epidemic of vitamin D deficiency, whose financial impact in the USA alone was estimated to be almost six times greater than the amount spent on diseases related to sun overexposure.
Get out of the sun!
Estimates of optimal sun exposure time vary depending on latitude, season, and individual skin characteristics. However, it is easy to know when the dose is excessive: the skin turns red. It is the reaction of erythema or sunburn, a natural protection mechanism selected during human evolution to avoid the consequences of excessive sun exposure. Skin redness means: get out of the sun!
Why? Because this reaction primarily arises as a physiological response to the absorption of UV-B radiation by DNA pyrimidine bases in skin cells, producing DNA photoproducts that activate an acute inflammatory response. These photoproducts also generate mutations that, depending on the affected proteins, increase the risk of developing skin cancer.
Sunscreen use avoids the erythemal reaction, but not the long-term consequences of overexposure to UV-A and VL. In addition, sunscreen blocks the beneficial effects of exposure to UV-B rays.
Moreover, the famous SPF - sun protection factor - is not a precise parameter as the measurement is performed on fair-skinned volunteers and uses only sources of UV-B irradiation. Consequently, SPF only considers protection against acute skin responses, ignoring all other positive and negative consequences of sun exposure. “Sadly, the belief that SPF properly defines and quantifies the efficacy of sun protection is nothing but another misconception, which still deludes health professionals and the general public”, the authors write.
Also, people with darker skin tones are dependent on test results that may not be fully applicable to them. Even the Fitzpatrick classification, which varies from type I to VI, from the lightest to the darkest skin, was created in the 1970s to estimate the tolerance to UV radiation of light-skinned people, and only later did it include other tones. The classification is based on responses to a simple questionnaire about the person’s previous experience with sun exposure (sunburn, tan, erythema, swelling, and discomfort and pain).
The amount of melanin, a pigment selected by evolution to protect human skin from sun exposure, is the determining factor for the absorption and dispersion of visible light by the epidermis and, therefore, contributes to the color of human skin. But even if they are less susceptible to UVB radiation, people with darker skin tones who are overexposed to the sun will face chronic problems in the long term, because the penetration of visible light is only partially reduced.
According to the researchers, the best way to improve sun protection strategies involves knowing the properties of the photosensitizers described in this work and the chemical and biological transformations induced by light, which can occur during and after exposure of human skin to the sun, with and without the application of currently used sunscreens.
“A deeper understanding of the interactions between sunlight and skin of different types will pave the way for innovative skincare strategies that not only involve avoiding the harmful effects but also consider the beneficial effects of sun exposure and the development of sun protection products tailored to specific skin types.“
The article Endogenous Photosensitizers in Human Skin, de Erick L. Bastos, Frank H. Quina and Maurício S. Baptista, can be accessed here.
